On a scorching hot morning in Vienna, the Sunday session of ERS kick-started with a highly interesting discussion covering cardiovascular disease (CVD) in chronic obstructive pulmonary disease (COPD).
Co-occurring comorbidities in COPD
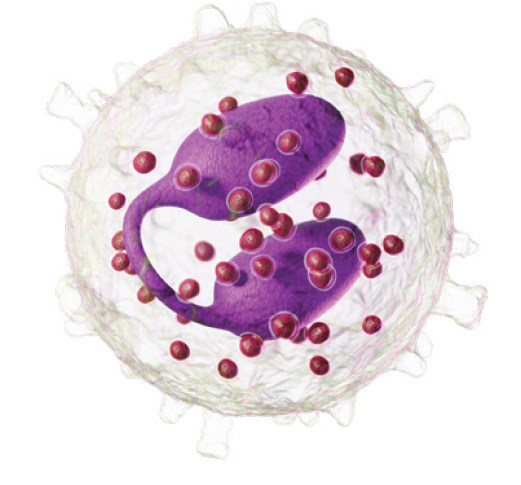
Individuals living with COPD often have several comorbidities. Prevalence of CVD in COPD is particularly high1 and is associated with an increased risk of death2. For example, COPD patients with mildly reduced ejection fraction have higher all-cause mortality than non-COPD patients with reduced ejection fraction3. Still, underdiagnosis of cardiovascular disease is high in patients with COPD.4
Every exacerbation matters
The association between CVD and COPD could be a consequence of shared risk factors (environmental and/or genetic factors), shared pathophysiological pathways, the co-occurrence of both diseases, and the adverse effects of COPD contributing to CVD, states Borja Garcia-Cosio. In clinical practice, controlling COPD is crucial, as a COPD exacerbation could trigger subsequent cardiovascular events. This risk remains elevated for up to a year after the exacerbation, and it intensifies with the severity of the episode5. Importantly, this increased risk is present even in patients who have not previously been diagnosed with CVD6. As Sami Simons stated: “Every exacerbation matters”.
If we do not look for it, we will never find it!
To address the underdiagnosis of CVD in COPD, early detection of CVD in COPD using a proactive search strategy is essential7. Several tools are available to determine CVD risk in the clinic8. For instance, CT thorax scans have been used to detect coronary artery calcification in COPD patients, which has been linked to increased dyspnea, reduced exercise capacity, and all-cause mortality9. Methods such as calculating risk scores with questionnaires, blood measurements (e.g., BNP, glucose, lipids), lung function testing, ECG, and echocardiogram also provide important clinical information that can identify individuals with high CVD risk and enable timely initiation of appropriate treatment says Bianca Beghè.
Addressing non-pharmacological or pharmacological
Treatment for COPD patients at risk of CVD may involve both non-pharmacological and pharmacological interventions. Jennifer Quint emphasizes the importance of non-pharmacological strategies, such as smoking cessation and physical activity, which have proven to be critical in reducing CVD risk.
Reduction in exacerbation and hospitalization risk, along with lung function improvement and better quality of life improvements has been demonstrated for triple therapy (ICS/LABA/LAMA)10-13, however impact on cardiovascular health and premature death still remains to be determined. Available post-hoc analysis14-16 of clinical trials have not been powered to demonstrate impact on all-cause mortality and since these studies are heterogenous and of explanatory nature, there is no clear evidence on all-cause mortality. However, Quint is optimistic that by combining real-world evidence with randomized controlled trials powered to address CVD risk and mortality, the evidence may become more robust in the future.
Shift in treatment
In clinical practice, a shift in perspective is needed when managing COPD patients. Improving diagnostic accuracy will require closer collaboration between pulmonologists and cardiologists, along with the development of holistic guidelines for managing multimorbidity in patients with complex chronic conditions. Early detection, phenotyping, and timely treatment are vital to reducing CVD risk in the COPD population.

Emil Bojsen-Møller
Medical Advisor, Chiesi Nordic
Primary care based integrated COPD disease management – are there benefits for the healthcare system?
Severe exacerbations in patients with chronic obstructive pulmonary disease (COPD) is a challenge for both patient and health care system. Methods to prevent exacerbations are therefore needed. A presentation on Sustained Läs mer
Biologics in COPD – are we there?
Current status of biologics in COPD In Professor Alberto Papi’s comprehensive lecture on the evolving landscape of biological treatment in COPD, he emphasized the proven efficacy of triple therapy in Läs mer
Update from the International Respiratory Coalition
Last congress morning, a much-changed Milan and ERS appeared: the temperature had dropped, there was light rain, the city smelled of flowers and green grass, and a scarcity of people Läs mer
References:
- Fabbri, L. M., Celli, B. R., Agustí, A., Criner, G. J., Dransfield, M. T., Divo, M., Krishnan, J. K., Lahousse, L., Montes de Oca, M., Salvi, S. S., Stolz, D., Vanfleteren, L. E. G. W., & Vogelmeier, C. F. (2023). COPD and multimorbidity: Recognising and addressing a syndemic occurrence. The Lancet. Respiratory Medicine, 11(11), 1020–1034. https://doi.org/10.1016/S2213-2600(23)00261-8
- Divo, M., Cote, C., De Torres, J. P., Casanova, C., Marin, J. M., Pinto-Plata, V., Zulueta, J., Cabrera, C., Zagaceta, J., Hunninghake, G., Celli, B., & for the BODE Collaborative Group. (2012). Comorbidities and Risk of Mortality in Patients with Chronic Obstructive Pulmonary Disease. American Journal of Respiratory and Critical Care Medicine, 186(2), 155–161. https://doi.org/10.1164/rccm.201201-0034OC
- Lau, F., Schupp, T., Schmitt, A., Reinhardt, M., Abel, N., Abumayyaleh, M., Weidner, K., Duerschmied, D., Ayoub, M., Mashayekhi, K., Akin, M., Ayasse, N., Akin, I., & Behnes, M. (2024). Prognostic impact of chronic obstructive pulmonary disease in patients with heart failure with mildly reduced ejection fraction. Respiratory Medicine, 223, 107536. https://doi.org/10.1016/j.rmed.2024.107536
- Kibbler, J., Wade, C., Mussell, G., Ripley, D. P., Bourke, S. C., & Steer, J. (2023). Systematic review and meta-analysis of prevalence of undiagnosed major cardiac comorbidities in COPD. ERJ Open Research, 9(6), 00548–02023. https://doi.org/10.1183/23120541.00548-2023
- Graul, E. L., Nordon, C., Rhodes, K., Marshall, J., Menon, S., Kallis, C., Ioannides, A. E., Whittaker, H. R., Peters, N. S., & Quint, J. K. (2024). Temporal Risk of Nonfatal Cardiovascular Events After Chronic Obstructive Pulmonary Disease Exacerbation: A Population-based Study. American Journal of Respiratory and Critical Care Medicine, 209(8), 960–972. https://doi.org/10.1164/rccm.202307-1122OC
- Yang, H., Ryu, M. H., Carey, V. J., Kinney, G. L., Hokanson, J. E., Dransfield, M. T., Hersh, C. P., Silverman, E. K., Crapo, J. D., Silverman, E. K., Make, B. J., Regan, E. A., Beaty, T. H., Castaldi, P. J., Cho, M. H., DeMeo, D. L., El Boueiz, A., Foreman, M. G., Ghosh, A., … Singh, H. (2024). Chronic Obstructive Pulmonary Disease Exacerbations Increase the Risk of Subsequent Cardiovascular Events: A Longitudinal Analysis of the COPDGene Study. Journal of the American Heart Association, 13(11), e033882. https://doi.org/10.1161/JAHA.123.033882
- Groenewegen, A., Zwartkruis, V. W., Rienstra, M., Zuithoff, N. P. A., Hollander, M., Koffijberg, H., Oude Wolcherink, M., Cramer, M. J., Van Der Schouw, Y. T., Hoes, A. W., Rutten, F. H., & De Boer, R. A. (2024). Diagnostic yield of a proactive strategy for early detection of cardiovascular disease versus usual care in adults with type 2 diabetes or chronic obstructive pulmonary disease in primary care in the Netherlands (RED-CVD): A multicentre, pragmatic, cluster-randomised, controlled trial. The Lancet Public Health, 9(2), e88–e99. https://doi.org/10.1016/S2468-2667(23)00269-4
- Polman, R., Hurst, J. R., Uysal, O. F., Mandal, S., Linz, D., & Simons, S. (2024). Cardiovascular disease and risk in COPD: A state of the art review. Expert Review of Cardiovascular Therapy, 22(4–5), 177–191. https://doi.org/10.1080/14779072.2024.2333786
- Williams, M. C., Murchison, J. T., Edwards, L. D., Agustí, A., Bakke, P., Calverley, P. M. A., Celli, B., Coxson, H. O., Crim, C., Lomas, D. A., Miller, B. E., Rennard, S., Silverman, E. K., Tal-Singer, R., Vestbo, J., Wouters, E., Yates, J. C., Van Beek, E. J. R., Newby, D. E., … for the Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) investigators. (2014). Coronary artery calcification is increased in patients with COPD and associated with increased morbidity and mortality. Thorax, 69(8), 718–723. https://doi.org/10.1136/thoraxjnl-2012-203151
- Lipson, D. A., Barnhart, F., Brealey, N., Brooks, J., Criner, G. J., Day, N. C., Dransfield, M. T., Halpin, D. M. G., Han, M. K., Jones, C. E., Kilbride, S., Lange, P., Lomas, D. A., Martinez, F. J., Singh, D., Tabberer, M., Wise, R. A., & Pascoe, S. J. (2018). Once-Daily Single-Inhaler Triple versus Dual Therapy in Patients with COPD. New England Journal of Medicine, 378(18), 1671–1680. https://doi.org/10.1056/NEJMoa1713901
- Papi, A., Vestbo, J., Fabbri, L., Corradi, M., Prunier, H., Cohuet, G., Guasconi, A., Montagna, I., Vezzoli, S., Petruzzelli, S., Scuri, M., Roche, N., & Singh, D. (2018). Extrafine inhaled triple therapy versus dual bronchodilator therapy in chronic obstructive pulmonary disease (TRIBUTE): A double-blind, parallel group, randomised controlled trial. The Lancet, 391(10125), 1076–1084. https://doi.org/10.1016/S0140-6736(18)30206-
- Singh D, Papi A, Corradi M, Pavlišová I, Montagna I, Francisco C, Cohuet G, Vezzoli S, Scuri M, Vestbo J. Single inhaler triple therapy versus inhaled corticosteroid plus long-acting β2-agonist therapy for chronic obstructive pulmonary disease (TRILOGY): a double-blind, parallel group, randomised controlled trial. Lancet. 2016 Sep 3;388(10048):963-73. doi: 10.1016/S0140-6736(16)31354-X.
- Vestbo, J., Papi, A., Corradi, M., Blazhko, V., Montagna, I., Francisco, C., Cohuet, G., Vezzoli, S., Scuri, M., & Singh, D. (2017). Single inhaler extrafine triple therapy versus long-acting muscarinic antagonist therapy for chronic obstructive pulmonary disease (TRINITY): A double-blind, parallel group, randomised controlled trial. The Lancet, 389(10082), 1919–1929. https://doi.org/10.1016/S0140-6736(17)30188-5
- Lipson, D. A., Crim, C., Criner, G. J., Day, N. C., Dransfield, M. T., Halpin, D. M. G., Han, M. K., Jones, C. E., Kilbride, S., Lange, P., Lomas, D. A., Lettis, S., Manchester, P., Martin, N., Midwinter, D., Morris, A., Pascoe, S. J., Singh, D., & Wise, R. A. (2020). Reduction in All-Cause Mortality with Fluticasone Furoate/Umeclidinium/Vilanterol in Patients with Chronic Obstructive Pulmonary Disease. American Journal of Respiratory and Critical Care Medicine, 201(12), 1508–1516. https://doi.org/10.1164/rccm.201911-2207OC
- Martinez, F. J., Rabe, K. F., Ferguson, G. T., Wedzicha, J. A., Singh, D., Wang, C., Rossman, K., St. Rose, E., Trivedi, R., Ballal, S., Darken, P., Aurivillius, M., Reisner, C., & Dorinsky, P. (2021). Reduced All-Cause Mortality in the ETHOS Trial of Budesonide/Glycopyrrolate/Formoterol for Chronic Obstructive Pulmonary Disease. A Randomized, Double-Blind, Multicenter, Parallel-Group Study. American Journal of Respiratory and Critical Care Medicine, 203(5), 553–564. https://doi.org/10.1164/rccm.202006-2618OC
- Vestbo, J., Fabbri, L., Papi, A., Petruzzelli, S., Scuri, M., Guasconi, A., Vezzoli, S., & Singh, D. (2018). Inhaled corticosteroid containing combinations and mortality in COPD. European Respiratory Journal, 52(6), 1801230. https://doi.org/10.1183/13993003.01230-2018
ID 10026-13.09.2024