Reference to presentation: Current challenges in airways disease management – Evolution in GOLD: we cannot ‘see’ ‘C’ anymore and LABA/ICS are gone. Helpful or a hindrance?
Speaker: Antonio Anzueto, USA
When the first GOLD guideline document was released in 2001, the assumption was that poorer lung function led to poorer outcome. The best strategy was therefore thought to be a step-up approach where more pharmacotherapy was added depending on the severity of the lung function reduction.
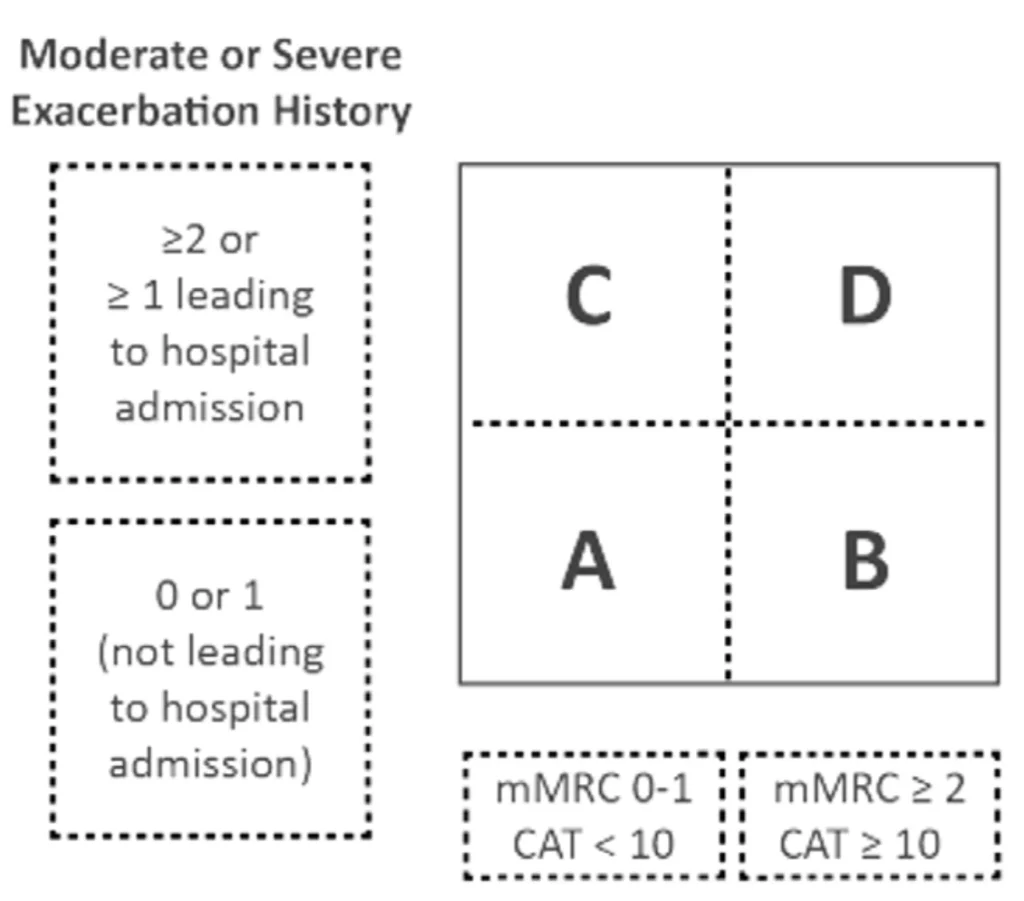
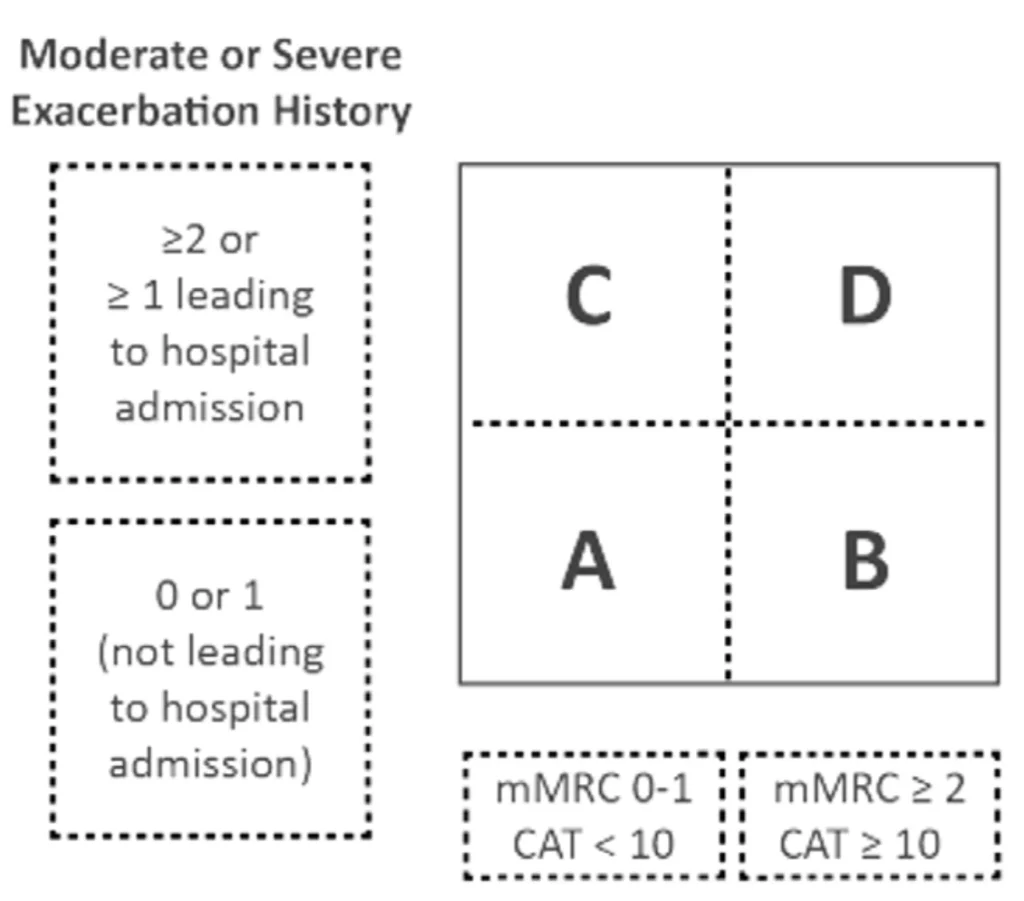
By 2015, data had accumulated showing that there was no association between the severity by lung function and symptoms evolution, risk of exacerbations or even outcomes. Data also clearly showed that there were means to prevent exacerbations and reduce symptoms. The GOLD committee decided to divide patients into four groups, ABCD (2015 Global Initiative for Chronic Obstructive Lung Disease).
Reference to presentation: Current challenges in airways disease management – Evolution in GOLD: we cannot ‘see’ ‘C’ anymore and LABA/ICS are gone. Helpful or a hindrance?
Speaker: Antonio Anzueto, USA
When the first GOLD guideline document was released in 2001, the assumption was that poorer lung function led to poorer outcome. The best strategy was therefore thought to be a step-up approach where more pharmacotherapy was added depending on the severity of the lung function reduction.
By 2015, data had accumulated showing that there was no association between the severity by lung function and symptoms evolution, risk of exacerbations or even outcomes. Data also clearly showed that there were means to prevent exacerbations and reduce symptoms. The GOLD committee decided to divide patients into four groups, ABCD (2015 Global Initiative for Chronic Obstructive Lung Disease).
Exacerbations – not just about lungs
It was not fully understood until recent years that exacerbations changes disease progression. It is now recognized that exacerbations are bad and should be prevented. They trigger more inflammations, accelerate decline in lung function, increase worsening of comorbidities1. Patients who are hospitalised due to exacerbation are significantly at risk for cardiac events within the next 30 days. Exacerbations should be viewed in the light of the intimate interaction between lungs and the cardiovascular system.
There is strong data evidence to justify replacing the CD category with just E for Exacerbation prone patients, irrespective of symptoms. Whatever interventions done, they must address exacerbation risk.
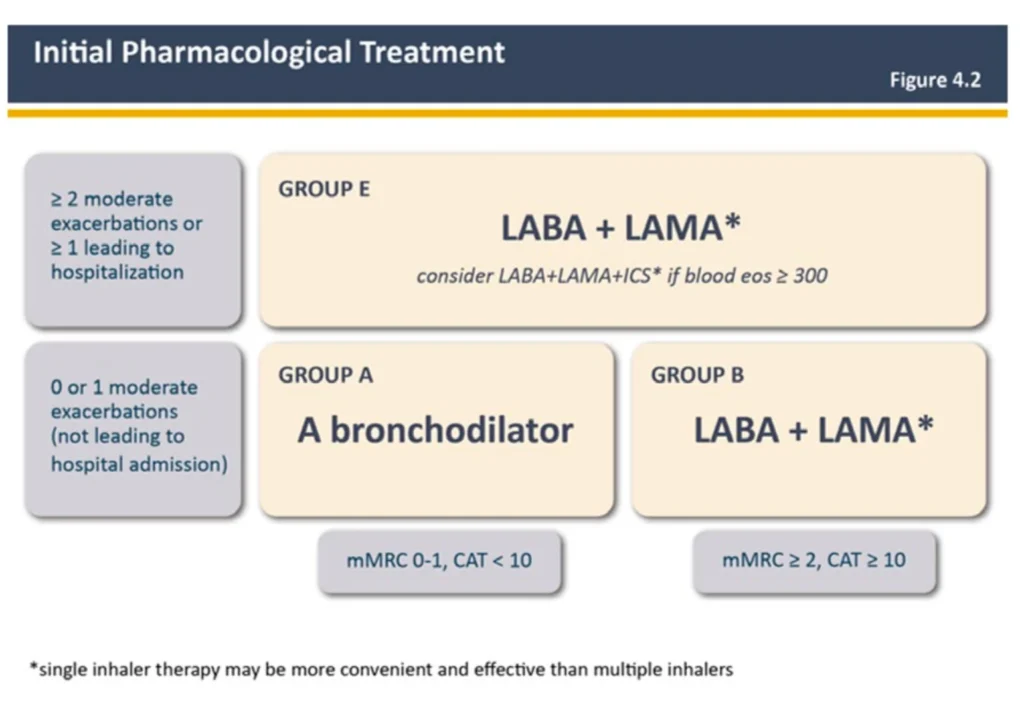
State of the art COPD treatment – according to GOLD 2023
Based on the large amount of data gained in recent years to understand the role of bronchodilators, the committee decided to make following changes in GOLD 2023 guideline:
– “Initial therapy should consist of a LAMA+LABA combination…”
– “Consider LAMA+LABA+ICS combination if eos >300 cells/μL (practical recommendation…”
– “We do not encourage the use of LABA+ICS combination in COPD…”
– “If patients have COPD and concomitant asthma, they should be treated like patients with asthma…”
Gold 2023:
There are several publications showing that fixed LAMA/LABAs are better than ICS/LABA in lung function and reducing exacerbations.2,3,4
Use of ICS
Safety issues: Patients on ICS based medications that are still not getting any clinical benefit, may have increased risk for pneumonia due to the change of the airway microbiome5. Eosinophils may serve as biomarkers to indicate risk of pneumonia: a very low eosinophil count (<100 cells/μL) marks an increased risk.6
Place in therapy: ICS, together with bronchodilators, are intended to give maximum bronchodilation and anti-inflammation. Programs including thousands of patients in registration studies have demonstrated that these medications decrease exacerbations7. Exacerbations are known to be key drivers for mortality in COPD8.
Take-home message
1. We live in the golden era of COPD. More treatments are available now, compared to 20 years ago. New molecules are being developed and there is also a potential for biologics. The prospects are huge.
2. Exacerbations are bad – independent of the patient’s symptoms.
– Dual bronchodilators are the pivotal therapy9
– ICS should be used only in the context of triple therapy9
– Therapies are shaped by biomarkers and treatable traits

Pekka Ojasala
Medical Advisor
References:
- Flattet Y, Garin N, Serratrice J, Perrier A, Stirnemann J, Carballo S. Determining prognosis in acute exacerbation of COPD. Int J Chron Obstruct Pulmon Dis. 2017;12:467- 475. Published 2017 Jan 31. doi:10.2147/COPD.S122382
- Wedzicha JA, Banerji D, Chapman KR, et al. Indacaterol-Gly- copyrronium versus Salmeterol-Fluticasone for COPD. N Engl J Med. 2016;374(23):2222-2234. doi:10.1056/NEJMoa1516385
- Cazzola M, Page C, Rogliani P, Calzetta L, Matera MG. Dual bronchodilation for the treatment of COPD: From bench to bedside. Br J Clin Pharmacol. 2022;88(8):3657-3673. doi:10.1111/bcp.15390
- Vogelmeier C, Paggiaro PL, Dorca J, et al. Efficacy and safety of aclidinium/formoterol versus salmeterol/fluticasone: a phase 3 COPD study. Eur Respir J. 2016;48(4):1030- 1039. doi:10.1183/13993003.00216-2016
- Contoli M, Pauletti A, Rossi MR, et al. Long-term effects of inhaled corticosteroids on sputum bacterial and viral loads in COPD. Eur Respir J. 2017;50(4):1700451. Published 2017 Oct 5. doi:10.1183/13993003.00451-2017
- Martinez-Garcia MA, Faner R, Oscullo G, et al. Inhaled Steroids, Circulating Eosinophils, Chronic Airway Infection, and Pneumonia Risk in Chronic Obstructive Pulmonary Disease. A Network Analysis. Am J Respir Crit Care Med. 2020;201(9):1078-1085. doi:10.1164/rccm.201908-1550OC
- See corresponding SmPC for exacerbation risk reduction per product
- Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, Salcedo E, Navarro M, Ochando R. Severe acute exacerbations and mortality in patients with chronic obstruc- tive pulmonary disease. Thorax. 2005;60(11):925-931. doi:10.1136/thx.2005.040527
- Global Initiative for Chronic Obstructive Lung Disease 2023 [cited Sept 2023]. Available from: http://www.goldcopd.com/
ID 345-2023-MARK (sept 2023)